Real-World Evidence
- In this section:
- Introduction

- Study Design

- Results

Introduction
The data presented below were gathered in a retrospective, real-world cohort study. Real-world evidence (RWE) provides data that can supplement the randomized clinical trial (RCT) findings, which remain the gold standard for evaluating the efficacy and safety of a treatment. Interpretation of the results are at the discretion of the audience as RWE data have inherent limitations.
Real-world evidence of XIFAXAN use: 30-day & annual rehospitalization due to OHE2
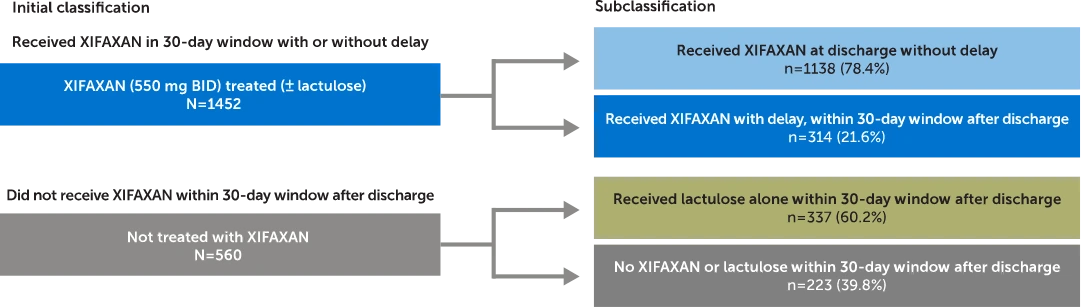
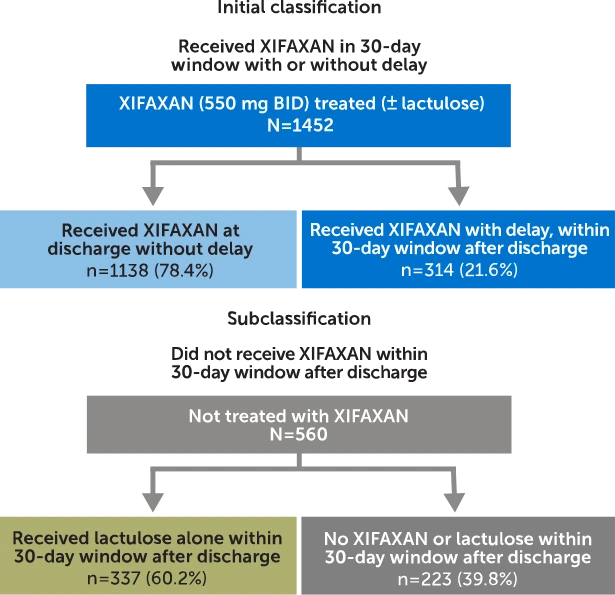
Patient classification based on treatment in the 30-day post-discharge window
Sample size and disposition
Commercially insured adults with an initial OHE hospitalization were identified and classified based on treatment received within a 30-day window after discharge and assessed for OHE rehospitalization and costs.
- OHE patients with ≥1 hospitalization* (N=3304)
- Adults 18-64 years old as of initial OHE hospitalization*,† (N=3162)
- Continuous health plan enrollment‡ (N=2012)
Study design
Claims analysis from MarketScan® Commercial Subset (October 1, 2015, through March 31, 2020). Patients were identified and classified based on treatment received in the 30-day post-discharge period. In patients who received XIFAXAN (± lactulose) within 30 days (N=1452), 78.4% (n=1138) received treatment at discharge (no delay). In patients who did not receive XIFAXAN within 30 days (N=560), 60.2% (n=337) of patients received lactulose alone.
Inclusion criteria: Adults (18-64 years old) with an initial overt OHE hospitalization* and continuous health plan enrollment‡
Exclusion criteria: Patients who had a liver transplant on or before the discharge date of the first OHE hospitalization were excluded from this study.
*Due to the lack of an OHE-specific ICD-10 code at the time of the study period to identify an OHE hospitalization in claims data, medical expertise was used to operationalize the definition of OHE hospitalization.1
†Also excluding patients who had a liver transplant on or before the discharge date of the first observed OHE hospitalization.
‡Continuous health plan enrollment ≥6 months prior to and ≥30 days after the first observed hospitalization.
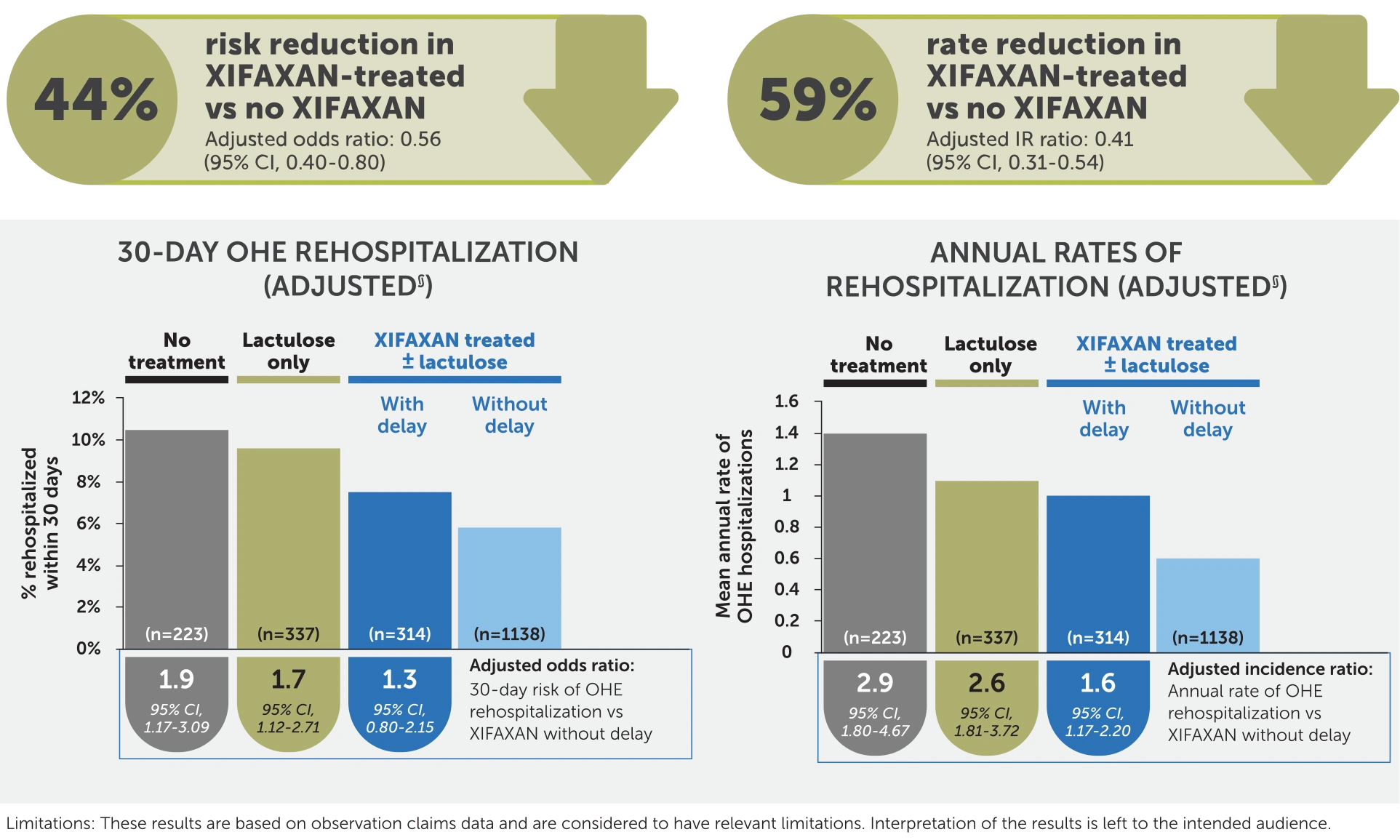
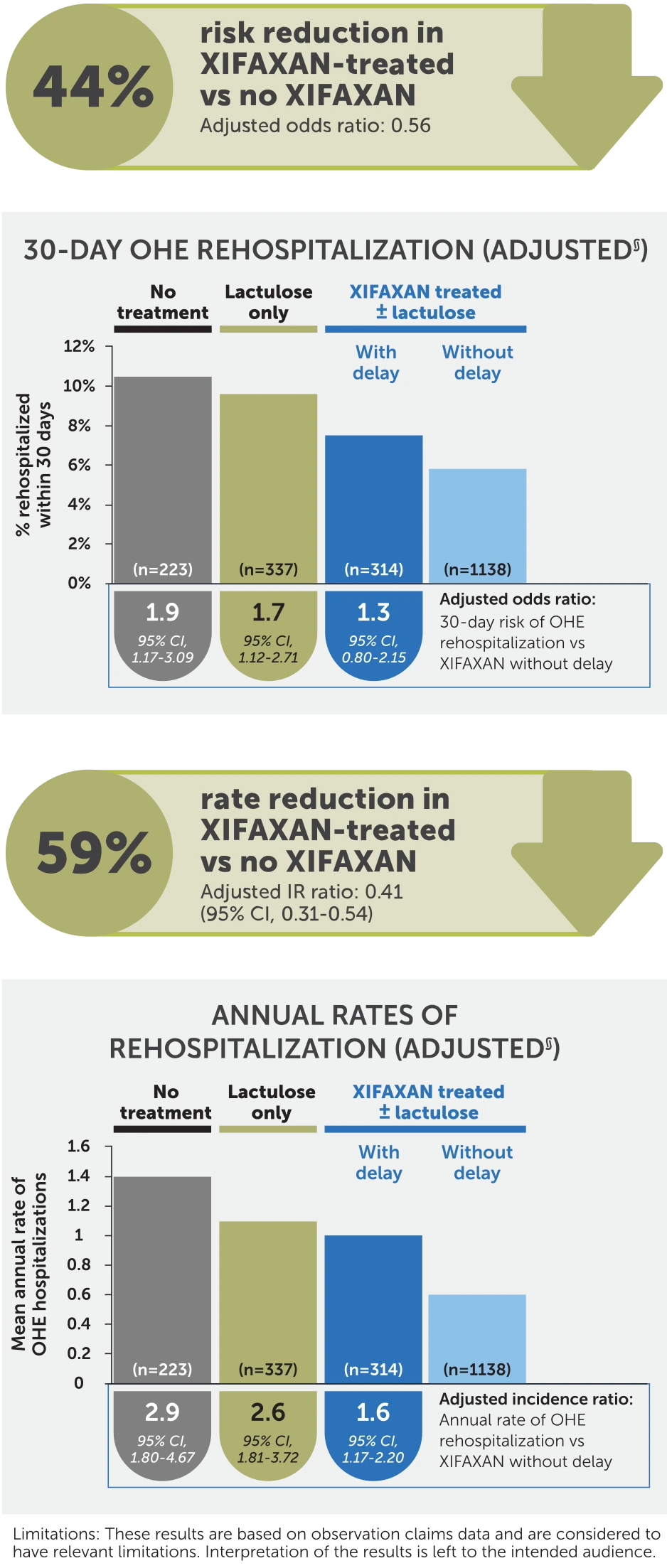
Observed reduction in OHE-related rehospitalizations with XIFAXAN2
Compared with patients given XIFAXAN without delay, other treatment subgroups showed increased odds of 30-day
risk of OHE rehospitalization and increased incidence of annual OHE rehospitalization
Study limitations
Results are based on observational claims data and are considered to have relevant limitations:
- Due to the retrospective design of the study, no causality can be established
- Claims data from commercially insured populations may not be generalizable to all patients with cirrhosis in the US and can contain omissions in coded procedures, diagnoses, and pharmacy claims
- Claims data contain limited clinical and laboratory information; as such, it was not possible to observe inpatient medications nor obtain patients’ cirrhosis severity (eg, MELD score, Child-Pugh grades)
- Despite adjustments for baseline characteristics in overt OHE hospitalization, residual selection bias and confounding may have remained
- Due to a lack of a specific ICD-10 diagnosis code for HE at the time the analyses were conducted, patients with HE were identified using an algorithm developed based on medical expert input
- For the purposes of this study, adherence was assumed to have been complete
- These real-world evidence study results are based on a retrospective cohort study of claims data with unequal group sizes. This imbalance may potentially affect the generalizability of the findings. The unbalanced number of patients per group may introduce biases
§Analyses were adjusted for a priori selected potential confounding factors associated with OHE hospitalization (ie, age, gender, health plan, region, cirrhosis-specific comorbidity scoring system score, prior gastroenterology consult, duration of index OHE hospitalization, treatment during baseline [eg, rifaximin, HE prophylaxis with antibiotics], indicators of portal hypertension [eg, varices], and factors associated with HE [eg, frailty index]).
IR, incidence rate; MELD, Model for End-Stage Liver Disease; OHE=overt hepatic encephalopathy.
References: 1. Gyawali B, Parsad S, Feinberg BA, Nabhan C. Real-world evidence and randomized studies in the precision oncology era: the right balance. JCO Precis Oncol. 2017;1:1-5. doi:10.1200/PO.17.00132 2. Jesudian AB, Gagnon-Sanschagrin P, Heimanson Z, et al. Impact of rifaximin use following an initial overt hepatic encephalopathy hospitalization on rehospitalization and costs. J Med Econ. 2023;26(1):1169-1177. doi:10.1080/13696998.2023.2255074
INDICATIONS
XIFAXAN® (rifaximin) 550 mg tablets are indicated for the reduction in risk of overt hepatic encephalopathy (HE) recurrence in adults and for the treatment of irritable bowel syndrome with diarrhea (IBS-D) in adults.
XIFAXAN® (rifaximin) 550 mg tablets are indicated for the reduction in risk of overt hepatic encephalopathy (HE) recurrence in adults.
IMPORTANT SAFETY INFORMATION
- XIFAXAN is contraindicated in patients with a hypersensitivity to rifaximin, rifamycin antimicrobial agents, or any of the components in XIFAXAN. Hypersensitivity reactions have included exfoliative dermatitis, angioneurotic edema, and anaphylaxis.
- Clostridium difficile-associated diarrhea (CDAD) has been reported with use of nearly all antibacterial agents, including XIFAXAN, and may range in severity from mild diarrhea to fatal colitis. If CDAD is suspected or confirmed, ongoing antibiotic use not directed against C. difficile may need to be discontinued.
XIF.0256.USA.24